The funny thing about “healing” is it looks different for everyone. I had this vision, or maybe a dream, of a blissful second pregnancy, one completely different than my first that would help me ‘heal’ from the traumas I experienced the first go around. Unfortunately, I never experienced bliss, but through the new obstacles, I did learn to connect with my mind and body in ways I never had before.
At the start of my pregnancy, I read a book called “Pregnancy Brain: A Mind-Body Approach to Stress Management During a High-Risk Pregnancy” by Parijat Deshpande which discussed a whole host of diagnoses associated with high-risk pregnancy and the power of our mind/body connection to help cope and overcome our odds. Now part of the reason I loved her book was that she was real, noting these methods don’t free you from pregnancy complications, however, they provide you with incredible tools to overcome whatever is thrown your way (and with it, the hope that the textbook outcomes won’t come true).
One of the strategies I loved was writing out your goals for pregnancy, no matter how small or large.
For me, my list was as follows:
- Be able to take maternity photos (something I had scheduled to do when I was pregnant with Zoey but never got the chance to because she came so early)
- Make it to 37 weeks pregnant (technically full term)
- Be able to hold my baby immediately after delivery (something I was unable to do with Zoey given the immediate attention she required to survive)
- Deliver a healthy baby who would room in with me and be discharged with us the same day we went home
Spoiler alert, I accomplished 3 out of 4 of these goals, so let’s start from the beginning.
Before getting pregnant, I started getting acupuncture and adjustments, something I had never done before, but after reading up on it, and discussing it with my provider, found this to be a great method for helping to get pregnant and hopefully stay pregnant. The combination of the two treatments would help keep my blood flowing correctly, help me manage my stress and swelling, and ensure my body stayed aligned to optimize my ability to grow a healthy human being.
Soon after these appointments started I got a positive pregnancy test and the journey began.
During my confirmation appointment, my OB mentioned he wanted to manage my pregnancy as if it was “normal” and not treat me as high risk unless something went wrong… *Noting he was planning to place a cerclage, but didn’t believe I needed any additional appointments or monitoring. Now being the type A person I am, and having gone through what I had with Zoey, I wasn’t about to take a reactive approach. I knew it wouldn’t be good for my mental or physical health and I didn’t agree with my OB’s course of action so I took the first step in learning to advocate for myself. Another important lesson in Parijat’s book. After my confirmation appointment, I requested to be seen by a Maternal Fetal Medicine (MFM) specialist.
At 10.5 weeks pregnant I met my MFM for the first time and we discussed our plan.
At 13 weeks, with my MFMs approval, we finally took the baby moon we had planned when I was pregnant with Zoey and traveled abroad to London and the French Riviera, hopeful that nothing would go wrong while we were abroad.
At 15 weeks I had my cerclage placed, where I was given a spinal and a stitch was placed to help keep my cervix closed. Note: I was diagnosed with cervical insufficiency (such a nice name) after going into preterm labor with Zoey and this was considered the best course of action to help keep me pregnant this time around.
At 20 weeks my stitch and my cervix were holding stable, but my growth scan showed small cysts on the baby’s brain, ones my doctor assured me would go away throughout pregnancy, but caused additional anxiety that needed managing.
At my 24-week appointment, my stitch was holding but my cervix had shortened to 2.5 cm, anything above 2.5 is considered normal and anything below can be cause for concern. Since I was right smack dab on the line, my MFM did not believe I needed any additional intervention, such as progesterone suppositories/shots, something I had read up on that can help keep your cervix strong and long in addition to the stitch.
Since I was nervous that things might get worse, I took matters into my own hands and started using an over-the-counter progesterone cream. I also cut back the level of activity I was doing, I had been going on 45-60 min walks a day, but quickly cut them down to 20 minutes and spent more time off my feet than I ever had before.
Outside of walking, I had quit working out altogether as soon as I found out I was pregnant, a difficult decision but one I knew was necessary to help keep the pressure off my cervix and this baby safe.
Looking back at that appointment I realize I wasn’t doing a good job managing my stress and anxiety. While I thought I had a good handle on things, I realize the days and weeks leading up to that 24w 3d milestone were a lot more difficult to “manage” than I had anticipated and I truly believe this also played a role in my cervix shortening during this time.
At my 26-week appointment my cervix was back up in the 3’s, I guess that’s what they mean when they say “dynamic cervix!” A huge sigh of relief and potential proof that what I was doing was working? And even more to celebrate because that meant I could more comfortably fly back east, again with my MFMs approval, for what was our last planned travel, to stand next to my best friend, while she married her best friend.
At 27 weeks I fired my OB and requested a transfer. In hindsight, I should have done this a lot sooner. He 1) As I mentioned above had wanted to treat me as a normal patient vs. high risk, seeing me only once a month and not placing any additional measures/checks throughout 2) When I went in for my appointments I would have to remind him of my history, he wouldn’t remember he had performed a small procedure on me the year prior, he wouldn’t remember I had a 24w 3d child, he wouldn’t remember I had been diagnosed with IC, he wouldn’t remember I had a cerclage placed, he wouldn’t remember I was seeing an MFM who worked in the same building, nor would he have the notes or records they’d been sharing reviewed ahead of my appointment. I’d find myself having the same conversations and explaining my situation over and over again until it got to the point where I’d had enough. I needed an OB who took the time to at least review my file before speaking with me, who made me feel heard and well supported, who could understand how I felt and could help assure me along the way. Another important piece shared in “Pregnancy Brain” ensuring you and your doctors are on the same page and you feel supported can go a long way in helping you stay pregnant.
At 28 weeks my cervix was still holding strong in the 3’s and I graduated to being seen every 3 weeks vs. every 2 with my MFM. A minor win in the sea of appointments that had become my new life.
At 32 weeks I started seeing my new OB, who also had a micro preemie, hers at 28 weeks. She was already 1000x better than my original OB, put my mind at ease, and could relate to the experience I was having.
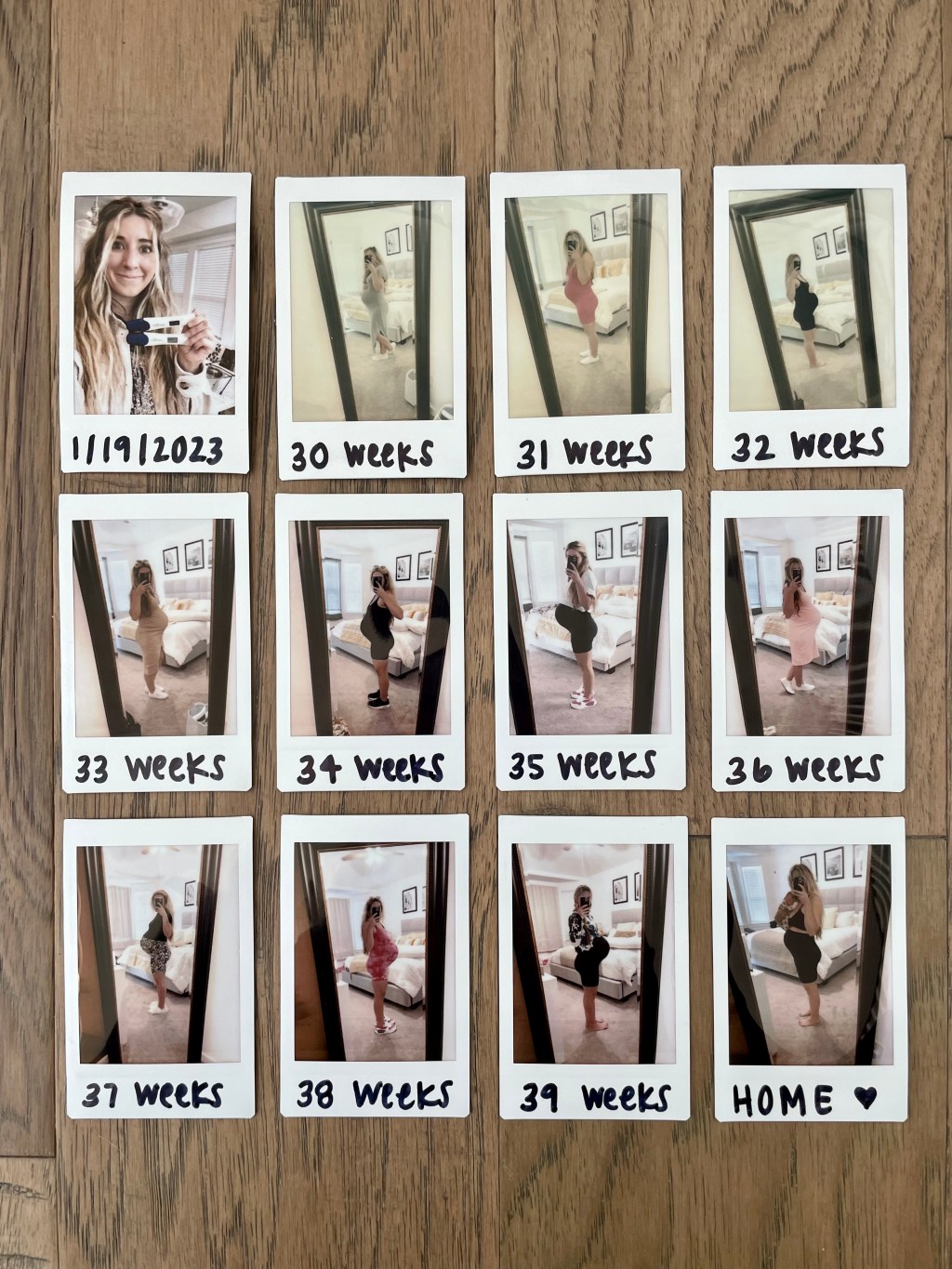
We also got our maternity photos done at 32 weeks (goal #1), a bit earlier than I had originally wanted, but my fear of going into labor before capturing this special time in our lives outweighed my desire to push them out any further.
At 36 weeks and 6 days, I had my cerclage removed! As my fellow ICers call it, ditch the stitch day, a day truly worth celebrating! Now I was convinced baby would come any day thereafter, heck I was already 2 CM dilated, despite my MFM predicting I’d go the full 40 weeks, so I held onto the high of making it to term the next day and the promise that the end was very near.
Then 38 weeks rolled around, and I’d hit my goal of making it to term (goal #2). I’d gone from 2 cm to 4 cm, but still no baby. I was uncomfortable, very over it, and ready to get this baby out!
Oh did I mention it was the hottest summer on record in Texas and I was the most pregnant during what were already known as the hottest months of the year? I had been avoiding the pool and baths, since I had my cerclage placed, due to the risk of infection, so to make matters even more fun my first time in the pool all summer long was at 38 weeks pregnant, in the middle of September…
At 38 weeks I tried my first session of induction acupuncture (I didn’t even know this was a thing!) and had my OB do a membrane sweep.
No such luck with either. So you can imagine my excitement when I hit 39 weeks, still no baby, getting more uncomfortable by the minute.
Hopeful, or maybe desperate, I scheduled one more induction acupuncture appointment.
Lo and behold, at 6:30 AM, the next morning, 39w 1d, I started having contractions. They were consistently ~3 minutes apart for an hour, and off to the hospital we went. While I was still only 4 cm dilated, I had a bulging bag and was admitted.
I waited for what felt like forever to get my epidural and by the time I got settled and more comfortable I was 6 cm dilated. However, it wasn’t until around 5 PM that the doctor came in and broke my water to help my labor continue to progress, and at 7 PM (12.5 hours later) I was finally 10 cm, 100% effaced, and ready to start pushing.
I pushed for 1.5-2 hours before we finally got to meet our baby. My husband got to do the honors of sharing our baby’s gender upon his arrival, it was a boy, Parker Austin!
Not finding out the gender of our baby was so special! A decision we made together, and one that was to provide us with some element of joy in the delivery room regardless of the outcome of this pregnancy.
Immediately after he was born he was put on my chest (goal #3), but he wasn’t crying so he was quickly swept off by the team and bagged to try and help him breathe. While the doctor was still focused on me and delivering the placenta and stitching me up (TMI, I know), I was watching the doctors attempt to get my son’s oxygen levels back up. When his SATs wouldn’t come back up the NICU was called and our hearts sank.
When the NICU doctor came up she confirmed what we’d been dreading. He’d need time in the NICU to help get what they believed to be fluid out of his lungs, a 3-4 day stay most likely. (Goal #4 slipped right through our fingertips).
However, when they assessed him more closely they noticed his pre and post-ductal o2 levels were giving drastically different numbers, meaning he most likely had pulmonary hypertension, a diagnosis vs. the initial “fluid in his lungs” thought. Outcome? More NICU time. More medication. More interventions.
That night he was given fentanyl, intubated to administer Surfactin, extubated, put on bubble CPAP, given a central line, had a chest x-ray and echo and was poked and prodded a million times. I of course was bedridden and not able to go see him until the morning.
No one talks about the kind of loneliness you experience when delivering a baby that needs NICU time. You lay in the bed you just delivered your baby in, perhaps still numb from the anesthesia, sore, in pain, and bleeding, while your partner escorts your baby to their new “home” for however long they’ll be there. All of the doctors, nurses and anticipatory celebration and excitement you’d been met with earlier are gone and you’re left alone to… wait.
Now with Parker’s new diagnosis, we were told he would most likely need a week, maybe 2 in the NICU, another punch to the gut, and to make matters more fun, I was discharged and sent home to wait, heal and rest as best I could.
Thankfully Parker was doing a lot better than the doctors anticipated over the course of the next five days; he was able to have his central line removed, be moved off of bubble CPAP to a high-flow nasal cannula, was able to start taking bottles by mouth, eventually came off of oxygen completely and before we knew it we were planning for his discharge on that 6th day.
While it wasn’t the outcome we had hoped for, it was a completely different experience than the one we’d had with Zoey, who spent 128 days in the NICU and we were elated to start our lives as a family of 4.
Now I’ll spare you the details of postpartum life with a newborn since for all intents and purposes my story ends with our baby coming home from the hospital.
But I’ll end with this.
When I mentioned this healing journey I was hoping to embark on was far from what I expected it, perhaps in some ways it was exactly what I needed. It was an experience that challenged my mind and body, that required me to put in the work, trust my body in ways I hadn’t before. It required me to learn new tools to cope and manage stress and anxiety, unlearn habits that hadn’t been serving me, slow down, make sacrifices and lean into the unknown.
It was an experience I had dreamed of, dreaded, loved, hated, and everything in between, and at the end of it, I got to meet our perfect new addition and walk away with a newfound appreciation for myself, my body, and the new found appreciation for my favorite saying “we can do hard things.”

Leave a comment